Patients, who live with their conditions daily, have invaluable insights that make them essential partners in developing effective treatments and building successful clinical trials. This is particularly the case for trials that incorporate electronic Clinical Outcome Assessments (eCOAs) as key endpoints and require increased patient engagement.
Early collaboration with patients’ representatives can help to design clinical that address real-world needs more effectively, leading to more relevant and significant research outcomes. This not only increases patient willingness to engage but also contributes to the development of treatments that truly benefit those who need them most.
Involving patients’ representatives in trial design also helps to ensure that the trial adheres to ethical guidelines, such as Good Clinical Practice (GCP), by integrating their perspectives on safety, consent, and burden. Recognized by regulatory authorities, this proactive approach can contribute to the overall success of the trial, by facilitating smoother regulatory approvals and oversight.
Throughout the trial and post-trial phases, direct engagement with the trial patients themselves becomes crucial. This ongoing collaboration with patients helps to maintain engagement, ensures clear communication, and facilitates the sharing of trial results in a patient-friendly manner.
Select the optimal collaboration format for each study objective
Depending on the stage of your study and your specific objectives, different approaches to patient engagement may be used, whether through patient representatives or trial patients themselves. Each format serves a distinct purpose in enhancing trial design, feasibility, and engagement.
Conduct patient advisory boards for early strategy and trial design
Boards patient representatives and advocates can help to gather initial insights. These boards can provide valuable feedback on trial design and strategy, ensuring alignment with patient priorities and addressing feasibility concerns. Evidence shows that early patient involvement leads to more relevant and feasible trial designs. This format is particularly useful during the early stages of planning.
Host focus groups to explore patient experiences
Organize discussions with diverse patient groups to understand their experiences, motivations, and expectations. Focus groups are more effective in the early stages, as they can help uncover a wide range of perspectives and potential barriers to participation. These group discussions can easily be held remotely, and many patient representatives appreciate being involved in this manner.
Conduct quantitative surveys for mid-study or late-stage real-time feedback
Use surveys, such as a Patient Feedback Questionnaire (PFQ) during the middle or late stages of a study to gather broader input from trial patients. These quantitative data help to identify why certain patterns emerge in participation or trial processes. When trials use electronic Clinical Outcome Assessments (eCOAs), PFQs can be seamlessly integrated to collect real-time feedback, enhancing patient engagement and the relevance of trial results.
Design patient-centric protocols
Working with patient representatives is essential for designing protocols that truly center around patient needs and preferences. Their involvement ensures that clinical trials are not only scientifically robust, but also considerate of patients’ daily lives.
Simplify Protocols
Reduce complexity and burden on patients. Protocols can be simplified using patient representatives’ insights, and simplified protocols can decrease patient dropout rates and improve compliance. Clear, straightforward procedures make it easier for patients to comply with study requirements.
Design flexible schedules
Design protocols that accommodate patients’ daily routines. Flexibility in visit schedules, treatment times, and follow-up procedures can reduce the disruption to patients’ lives. This makes participation more appealing and manageable for a diverse population.
Develop patient-friendly materials
Develop easy-to-understand consent forms and informational documents. Simplifying these materials ensures that patients fully grasp the trial’s purpose, risks, and benefits, leading to informed and enthusiastic participation. Engaging patients in this process has been shown to result in more practical and patient-friendly protocols.
Identify relevant endpoints
Collaborate with patient representatives to focus on what matters the most, and determine meaningful endpoints for the trial, ensuring that the outcomes measured are truly relevant to patient experiences and priorities:
- Incorporate Patient-Reported Outcomes (PROs) when you want to capture patients’ perspectives on their health status and quality of life. These outcomes provide direct insight into how treatments affect patients’ daily lives. Examples include symptom relief, physical functioning, and emotional well-being. Trials incorporating PROs often generate valuable data that help to determine the risks and benefits of treatments for patients. Additionally, PROs have proven to be effective tools in safety evaluations and can even more accurately reflect adverse events than physician-observed symptoms.
- Include Observer-Reported Outcomes (ObsROs), that is to say, outcomes reported by caregivers or others observing the patient when patients cannot reliably self-report, such as in pediatric or cognitively impaired populations. This ensures that the trial captures a full picture of the treatment’s impact. In more complex cases, such as rare diseases, where symptoms and challenges may not be fully understood, ObsROs can be particularly valuable in providing insights into aspects of the disease that may otherwise go unreported or unnoticed by the patient themselves.
- Utilize Performance Outcomes (PerfOs) to measure patients’ abilities to perform specific tasks. Common measures tracked through connected devices include timed walking tests, cognitive tasks, physical activity levels, and sleep patterns, offering comprehensive insights into patients’ functional health. PerfOs provide objective data on how treatments improve or impair patients’ functional abilities.
- Capture Clinician-Reported Outcomes (ClinROs), which consist of assessments made by healthcare professionals based on their observations and clinical judgement. ClinROs can complement PROs where they are available and provide essential data when patients are unable to complete questionnaires, ensuring comprehensive data collection. For example, in neurodegenerative diseases like ALS, where patients may progressively lose the ability to communicate, ClinRos are critical for tracking motor function decline, respiratory capacity – assessments that in some cases not only require specialized medical expertise but may also involve specific rater training to ensure consistency and accuracy.
Improve your recruitment and retention strategies
To optimize recruitment and retention, it’s crucial to engage both patient representatives and study patients themselves. While patient representatives can help to develop effective recruitment and retention materials, real-time feedback from trial patients is equally important. This allows for quick adjustment if recruitment is challenging or retention rates are low.
Co-create recruitment & retention materials with patient representatives
Develop materials with input from patient representatives to ensure clarity and appeal. Recruitment brochures, advertisements, and online content should address common patient concerns and motivations. Supportive materials, such as videos or PDFs, developed in collaboration with patient representatives, should be used throughout the study to reinforce patient engagement and retention. This approach makes recruitment and retention efforts more effective and trustworthy.
Work with patient ambassadors to ensure ongoing support and engagement
Employ patients to share their experiences and encourage participation. Ambassadors can provide peer support and credibility, easing the fears and uncertainties of potential participants. This personal touch can significantly boost recruitment and retention rates.
Establish feedback mechanisms
Establish channels for ongoing patient feedback during the trial. Regular feedback helps identify and address issues promptly, maintaining patient satisfaction and engagement. This continuous improvement loop enhances the overall trial experience for patients. This feedback can be provided via the Participant Feedback Questionnaire, where patients can express their feelings, e.g. about their experience of the study procedures, systems used, or clinical staff.
Ensure continuous communication with the trial patients throughout
Once the trial is live, maintaining consistent communication with trial patients is key to ensuring their engagement and satisfaction. This is also where tools such as the Participant Feedback Questionnaire can be used to gather insights and address any issues as they arise.
Provide regular updates
Provide your trial patients with updates through newsletters or informational letters. Sharing newsletters with patients can be facilitated by site staff to keep the patients informed about the trial’s progress and any changes. This transparency fosters a sense of involvement and trust, which is crucial for maintaining engagement.
Engage in two-way communication
Facilitate platforms such as dedicated hotlines, or email support for patients to ask questions and share concerns. Open lines of communication help address issues and reinforce the partnerships between patients and researchers. This responsiveness can improve patient satisfaction and adherence.
Acknowledge contributions
Recognize and appreciate patient involvement. Publicly acknowledging patient contributions through thank-you notes, certificates, or mentions in publications shows that their input is valued. This recognition can enhance patients’ sense of ownership and commitment to the trial.
Analyze and share results with trial patients post-trial
Collaborating with patients does not end when the study concludes. It’s crucial to thank patients for their involvement and continue engagement by sharing trial results. This also presents an opportunity for “lessons learned” by revisiting patient representatives who were engaged at the start of the trial, thereby finalizing the feedback loop.
Create patient-friendly summaries
Create summaries of trial results that are easy to understand. Simplified summaries ensure that patients can grasp the significance of the findings and how they contribute to medical knowledge. This transparency helps build trust and credibility.
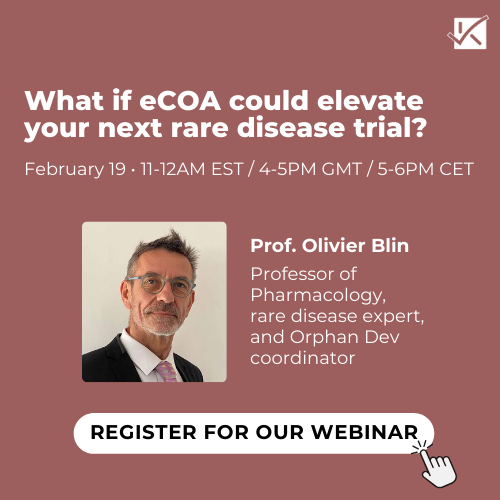
Organize results-sharing sessions
Host webinars or face-to-face meetings to discuss findings with patients. Interactive sessions allow patients to ask questions and provide feedback, fostering a collaborative atmosphere. This engagement can enhance patients’ understanding and appreciation of the research.
Share feedback on findings
Gather patient feedback on the implications of the trial results. This can be done through follow-up surveys or feedback sessions. Understanding patients’ perspectives on the outcomes can provide valuable insights for future research. This feedback loop ensures that patient priorities continue to shape clinical research.
Thank the patients
Show consideration by thanking patients at the end of the trial. A thank-you note, which is simple to implement, demonstrates appreciation for their participation and contributions.
Collaborating with patients and their representatives should be prioritized at every stage of the clinical trial, from initial design to post-trial analysis. This approach not only improves the ethical standards and relevance of the research, but also directly addresses the needs and experiences of the patients themselves. Moving forward, the key is to embed these structured steps as standard operating procedures across the industry, fostering a patient-centric culture that values and integrates patient insights as a core component of clinical research. This direction promises not only to enhance patient satisfaction and participation rates but also to produce reliable and actionable data, ultimately driving the development of treatments that truly improve patient outcomes and quality of life.